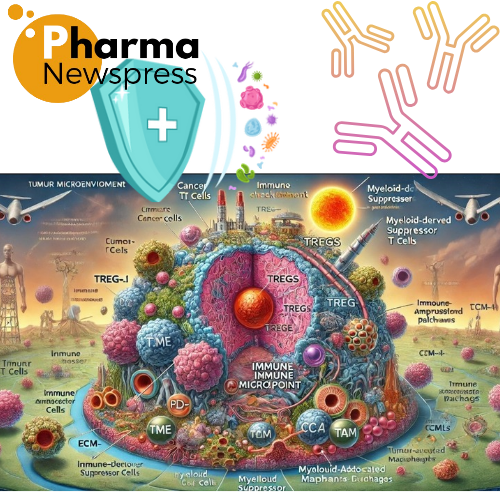
The tumor microenvironment (TME) is indeed a critical determinant of cancer progression and immune evasion. Its dynamic and immunosuppressive nature allows tumors to adapt and thrive in hostile conditions, making it a key focus for developing novel therapeutic strategies.
Key Mechanisms of TME Reprogramming:
- Recruitment of Immunosuppressive Cells:
- Regulatory T Cells (Tregs): Suppress effector T cell functions through cytokine secretion (IL-10, TGF-β) and direct cell-cell interactions.
- Myeloid-Derived Suppressor Cells (MDSCs): Inhibit T cell activation and proliferation, contributing to immune tolerance.
- Tumor-Associated Macrophages (TAMs): Often polarized to an M2-like phenotype, promoting tissue remodeling, angiogenesis, and immune suppression.
- Immune Checkpoint Pathways:
- Tumor cells upregulate immune checkpoint molecules like PD-L1 and CTLA-4, which bind to receptors on T cells, impairing their activation and promoting exhaustion.
- The TME further amplifies this by fostering conditions that enhance checkpoint molecule expression.
- Metabolic Reprogramming:
- Tumor cells shift to glycolysis (Warburg effect), depleting glucose and generating lactate, which impairs T cell function.
- Essential nutrients like tryptophan are depleted, and metabolic byproducts like kynurenine suppress immune activity.
- Hypoxia and Angiogenesis
- Hypoxia, driven by inadequate blood supply, stabilizes HIF-1α, upregulating VEGF and other factors that promote abnormal angiogenesis.
- Hypoxia and abnormal vasculature hinder T cell infiltration and create an immunosuppressive niche.
- Extracellular Matrix Remodeling:
- ECM stiffening and altered composition act as physical barriers to immune cell infiltration.
- Components like collagen and hyaluronic acid impede T cell migration and enhance tumor protection.
Therapeutic Opportunities:
- Reversing Immunosuppression:
- Targeting Tregs, MDSCs, and TAMs with small molecules or monoclonal antibodies to enhance immune cell activity.
- Combination therapies integrating immune checkpoint inhibitors (e.g., anti-PD-1, anti-CTLA-4) with agents targeting immunosuppressive cells.
- Metabolic Normalization:
- Intervening in glycolytic pathways or replenishing depleted nutrients to support T cell function.
- Targeting enzymes like IDO1 (indoleamine 2,3-dioxygenase) to reduce tryptophan depletion.
- Anti-Angiogenic Therapy:
- Using agents like bevacizumab (anti-VEGF) to normalize tumor vasculature and improve immune cell infiltration.
- Modulating hypoxia pathways to counteract the immunosuppressive effects of HIF-1α.
- ECM Remodeling:
- Enzymes such as hyaluronidase can degrade ECM components, reducing physical barriers to immune cells.
- Strategies to modulate ECM stiffness and composition are being explored.
- Combination Immunotherapy:
- Pairing CAR-T cell therapies or cancer vaccines with strategies that remodel the TME can enhance their efficacy.
Understanding the interplay between the TME and immune system continues to inform the development of more precise and effective cancer treatments. Transforming the TME from a shielded niche into a pro-inflammatory, immune-accessible environment is a cornerstone of next-generation immunotherapy.